Click here to read it in Marathi: भूल घेताय? सावधान!
This article is written to raise the public awareness about Pseudocholinesterase deficiency, a genetic condition in which a person lacks a protein required to break down some anesthetic drugs. Due to this inability to break down the anesthetic drug, the person remains paralyzed for a long time.
Before I talk about this Pseudocholinesterase deficiency, let me tell you the background on how anesthesia is given before surgery or a procedure is done. Initially, the patient is given some anesthetic drugs to make him unconscious. Then, the drug is given to paralyze him until surgery finishes, called muscle relaxants. The muscle relaxants can be short-acting or long-acting. Anesthesiologist selects either short acting or combination of both types of muscle relaxants based on how long the surgery is. Once a person is paralyzed, the tube is placed in his windpipe (trachea). The tube is then connected to the anesthetic machine, and the patient is given artificial respiration. In some rural areas, when machine is not available, the anesthesiologist gives mechanical ventilation manually (by using bellows). The most commonly used short-acting muscle relaxant is Succinylcholine chloride. It lasts for only a few minutes. Our body breaks it down with the help of one enzyme (protein) called Pseudocholinesterase.
Today, I will tell you about the genetic condition where this enzyme (protein) called Pseudocholinesterase is either not sufficient or absent due to the defective gene. As you can easily guess, persons with this condition remain paralyzed for a long time as the muscle relaxant does not get cleared from the body immediately.

I was a freelance anesthesiologist when I lived in India. It was my first year of anesthesiology practice. One day, I got a call from a senior anesthesiologist colleague and a surgeon. They asked me to come to their operation room immediately. When I reached there, they told me that one of their patients was not coming out of anesthesia. The patient was expected to recover from anesthesia within a few minutes after surgery was over. But the patient remained paralyzed for over one and a half hours after the surgery, and there were no signs of any recovery. They tried their best, but could not find what went wrong. As it was a small place, the anesthetic machine was not available, and the anesthesiologist was giving artificial breathing to the patient manually. I confirmed that the patient belongs to the Arya Vaishya community.
Since I had seen such a case before, I quickly guessed what was happening. I told them that it could be the genetic condition commonly seen in the Arya Vaishya or Komati community and I recommended giving the patient blood from someone who did not belong to that community. Luck was on my side, and my guess was correct! After receiving the blood, the patient recovered completely. His body used Pseudocholinesterase from the donor blood to break down Succinylcholine. I received a big pat on my shoulder from my anesthesiologist colleague and the surgeon! After this incident, I encountered two more similar cases during my anesthesiology practice and we managed them efficiently.
Now, I will share how I learned about this condition for the first time. My elder sister was supposed to have a tonsil surgery done in another city, Latur (Maharashtra, India). I was a first-year medical student, so at that time I did not have much knowledge of anesthesia drugs. Being that I was a medical student, the anesthesiologist and surgeon allowed me to be with my sister in the operating room during her tonsil surgery. As mentioned above, the anesthesiologist made my sister unconscious, gave her muscle relaxant before placing the tube in her windpipe. Her operation finished in less than 30 minutes, and guess what, my sister remained in that state for an extended period of time. They tried all possible ways to treat her and to find out the cause, but had no success. Almost one hour elapsed and still there was no signs of recovery. The anesthesiologist was very experienced. He came to us and told us that she might have a rare genetic condition that could keep her paralyzed for a long time. He then told us that she needed blood. I immediately told him that I could donate my blood to my sister, however, he stated that he does not want blood from her relatives but he preferred using blood from someone who did not belong to our (Arya Vaishya/Komati) community. She completely recovered after receiving blood, and we all breathed a sigh of relief! Later during my anesthesiology practice, that experience helped me save the lives of my patients with similar conditions (Honestly, I did not have any idea that I would be an anesthesiologist in the future 😊).
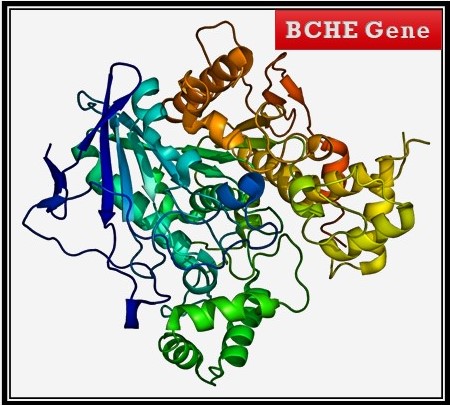
Now, let’s learn about this genetic condition. This condition is called pseudocholinesterase deficiency. Mutations in the BCHE gene can cause inherited pseudocholinesterase deficiency. It is seen in 1 per 2000 to 5000 people.
This gene provides instructions for making the pseudocholinesterase enzyme, known as butyryl cholinesterase. This enzyme is made by the liver and circulates in the blood. It is involved in breaking down (metabolizing) choline ester drugs. Mutations that cause pseudocholinesterase deficiency might impair the function or production of butyryl cholinesterase. If a person has one copy of a mutated (defective) gene, he is referred to as a carrier. If a person gets defective copies from both parents, they are affected. The carriers also take longer time to clear choline ester drugs but not as long as those with two mutated copies of the gene. Consanguinity, which means marriages in blood relations, can increase the risk of inheriting this condition. When two carriers of an autosomal recessive condition have children, each child has a::
- 25% chance to have the condition
- 50% chance to be an unaffected carrier like each parent
- 25% chance to be unaffected/normal

This condition is commonly seen in the Arya Vaishya community in India. It is also found in Jewish, Persian, Multani from Pakistan, Japanese, Egyptians, Iranians, Afghans, and Europeans. People with this genetic condition should avoid Succinylcholine and Mivacurium as well as local anesthetics (cocaine, procaine, benzocaine, tetracaine).

I know that it is tough to remember these names of enzyme and genetic condition. Just keep in mind that if anyone from Arya Vaishya community is going for surgery or dental procedure, which needs local anesthetic agents, let your doctor know that you belong to this community which has increased risk of one genetic condition where they take very long to recover from anesthesia or muscle relaxants.
If anyone has had such an experience (an episode of prolonged respiratory paralysis following general anesthesia), a blood test of the enzyme is available for them and their relatives. If someone dies during the operation and the cause of death is not found, their relatives should undergo this test. Patients with known pseudocholinesterase deficiency may wear a medic-alert bracelet that will notify healthcare workers of increased risk from the administration of Succinylcholine. They should warn their relatives to be tested before surgery since the condition is often inherited.

Sometimes this condition can be acquired, which means non-genetic. Pseudocholinesterase deficiency can result from chronic infections, kidney or liver disease, malnutrition, cancer, or pregnancy. Certain drugs can also reduce the production of the enzyme. You would not want you or your family members to be in a position of not knowing if something went wrong with anesthesia or if it was Pseudocholinesterase deficiency. Talk to your doctor about getting your Pseudocholinesterase levels checked by a blood test. Prevention is better than a cure!
Proofread by- Kerrian Duncan, an educator, Human Resources professional. Thank you, dear Kerrian.
Very nicely eloborated Savi
Thank you.
It is so nicely explained and easy to remember treatment part also.Great!
Thank you.
Excellently written article. It is clear and effective and I feel that I learned something important. Thank you and great job!
Thank you.
Very interesting information .
Thank you.
Very nice good effort to bring awareness
Thank you.
Very important information
Thank you.
A very new(for me)and important thing to know.Thanks for spreading awareness about it🙏
Thank you.
Well Dr. Bandari, you did it again! This information is new to me. It was jaw dropping as I read and read and continued reading. The use of the word paralyzed scared me. I was unaware of what actually happens during a procedure/ surgery. Once again Dr, thank you!
Thank you.
I am so glad to see that someone has been able to identify this medical problem. I am a affected person with this problem. I was tested back in 1970s when some of our female relatives ran into that problem after surgery. My mother tested all of us kids 4 boys and 1 girl and me the only girl is affected. I had 2 girls which are now adults and have their own children they are aware of the situation with me, and also have passed on the information to my grandkids doctors. Because I lost the test results and moving so much over the years I have had a hard time trying to explain the situation and get the proper testing done to find out if my kids or grandkids are affected with this missing Gene. The drug is also called Anectine/ Careerie. I do were a medical alert bracelet at all times. And just a note to you that I am not a part of any of the ethnic or genetic communities that you have listed from above and I am born and raised in the USA. My genetic is makeup or family background is French, Irish, Italian and English. Thank you so much for your article now hopefully I will be able to get the rest of my family tested so we will no longer have to worry about the problem as my family grows.
Thank you so much for your sharing your experience. I am glad that you found this article/information useful. It is interesting to know that it can be seen in other ethnicity other than I mentioned there. It would be interesting to see the actual test result. Thank you again for taking time to read and leaving the detailed comment.
I’m allergic to succinylcholine chloride also. I was given it as a baby for surgery. Was in cardiac arrest for a very long time and barely survived. I do have all my genetic records from Seattle’s children’s hospital. I believe my great grandmother had this allergy also. Ive tried to test my daughter but my doctor told me that my husband would have to be a carrier for her to have this mutation. I dont know if thats accurate. Anesthesiologist always get excited when they hear what I’m allergic too!
Thank you for sharing your experience. Allergy to succinylcholine chloride is different than this genetic condition where you do not have protein to break it. This genetic condition is autosomal recessive, means both parents have to have defective gene. Thank you again 🙂
Thank you so much for this article. I do have this condition, and wear a pseudo-cholinesterase medic alert bracelet. Both of my parents are carriers, and have not had any complications during their surgeries. We learnt of our allergy as children when my sister went into a coma after having her tonsils taken out. She survived, and we were tested. Now, as an adult I am getting a tonsillectomy and am curious if you have any suggestions about important questions to ask the anesthesiologist? I’ve been trying to research which anesthetic/s are used for someone with this allergy but haven’t been able to find anything, only what to avoid. Again, thanks so much.
Thank you for reading the article and sharing your experience. I am glad to know that your sister survived from coma. I’d suggest you not to worry about what other anesthetic drugs can be used. You just let your anesthesiologist know that you have this condition and they will do their job. There are many other anesthetic drugs as alternatives. No worries at all. Hope it helps.