
To read this article in Marathi, click here: मायग्रेन/अर्धशिशी
Headaches are a common health problem. A migraine is not just a bad headache. It is a disabling neurological condition that includes episodes of headache, that can last for several hours or several days, associated with other symptoms. Before 12 years of age, the prevalence of headaches is similar among males and females. After age 12 years, the prevalence is higher in females. In adults, migraine headaches are three times more common in women than in men. In 50% of cases, it begins before 20 years of age.
Many women experience migraines related to the hormonal changes of menstruation, oral contraceptives, pregnancy, post-partum (after childbirth), and menopause.
A family history of migraine is present in 70-80% of sufferers. So having a relative with migraines makes it more likely that you will have a migraine as well.
Migraine characteristics include:
- Pain typically on one side of the head (but in children, it can be on both sides of head)
- Pain has a pulsating or throbbing quality
- Moderate to intense pain affecting daily activity
- Nausea or vomiting
- Sensitivity to light and sound
- Attacks last 4 to 72 hours or longer in adults and 2-72 hours in children
- Exertion (e.g., climbing stairs or running) worsens the headache
There are three types of migraine:
- Migraine without aura (previously known as common migraine) is the most common type of migraine. Migraine attack starts without any warning signs.
- Migraine with aura (previously known as classic migraine) is seen in 20% of cases of migraine. Aura is a warning sign in the form of visual disturbances (e.g., wavy lines, dots, flashing lights, blurry vision, and blind spots) or disruptions in smell, taste, or touch from 20-60 minutes before the onset of a headache. In basilar migraine (now known as migraine with brainstem aura), person experiences speech difficulty, vertigo, balancing problem or ringing in the ear during aura.


- Atypical migraine– rare and exclusively seen in children. it can be seen in the first year of life! They usually do not have headaches but present with symptoms like vomiting, belly pain, or other symptoms. Examples include Cyclic vomiting syndrome, abdominal migraine, Alice in Wonderland syndrome, confusional migraine, etc.
What causes migraines? The exact cause of migraine is not known, but genetics and environment do play a role. There are different theories about how migraine happens. Many researchers believe that migraine sufferers have inherited a more “sensitive brain” than those without migraines. When a person gets exposed to loud noise, bright light, or excessive motion, he can adapt to these strong stimuli within minutes. But in people with migraines, due to a “sensitive brain,” it leads to a migraine attack. During a migraine attack, changes in brain activity cause release of certain chemicals. These chemicals activate pain pathways and also lead to inflamed blood vessels around the brain. Due to a lack of ability to adapt, a migraine attack can be provoked by bright light, excessive noise, strong smells, excessive motion, and painful stimuli.
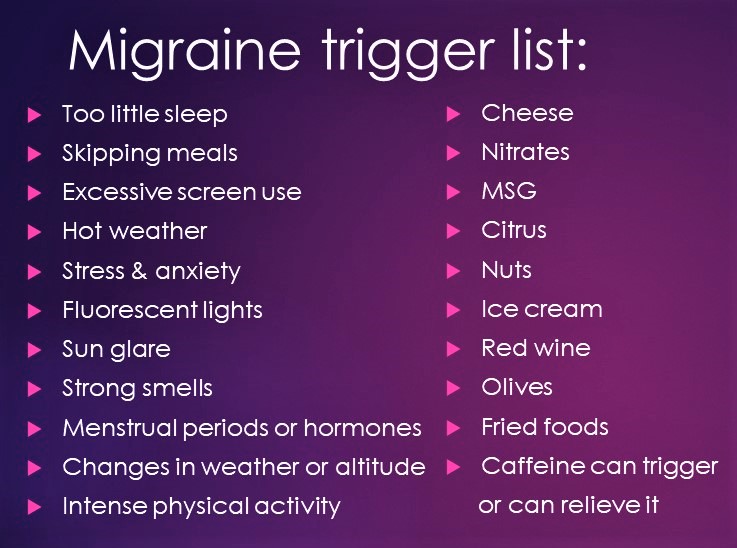
Migraine triggers can be hormonal, food, and other external factors.
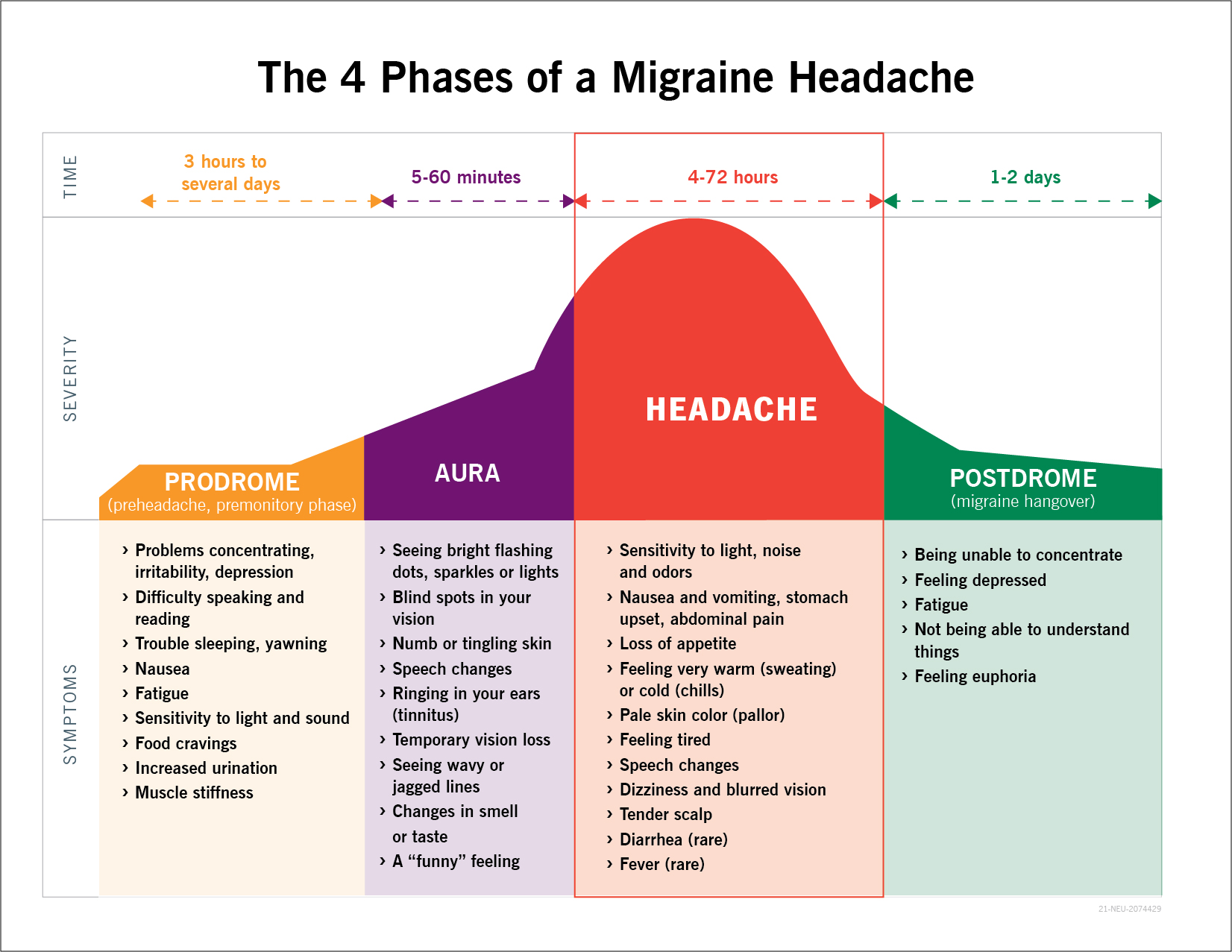
How is migraine diagnosed? Migraine is a clinical diagnosis. Based on your signs, symptoms, and neurological examination, a diagnosis can be made. There is no blood test or scan (ultrasound, CT scan, or MRI) or EEG (electroencephalogram or brain wave study) needed for migraine. If there is any suspicion of other causes, then you will need other tests or scans. There are 3-4 phases of a migraine. A typical migraine attack without aura progresses through three phases: the premonitory phase, the headache phase, and the postdrome phase. In migraine with aura, the aura is an additional phase that may occur before or with the headache.
Complications of migraine:
- Chronic migraine: Person gets 15 or more days per month of headache with migrainous features.
- Status Migrainosus: Usually, migraine attack lasts for maximum 72 hours. If it persists beyond 72 hours/3 days, it is called Status Migrainosus.
- Persistent aura without infarction: Usually aura lasts for 20-60 minutes. If it persists beyond 60 minutes but does not cause stroke, it is called persistent aura without infarction.
- Migrainous infarction/stroke: Persistent aura leads to stroke. This is a rare complication that happens mostly in younger women. Women under 45 who smoke and take birth control pills are at high risk.
- Migraine triggered seizure (migralepsy): is the term used when a seizure occurs during or within 1 hour of a typical migraine aura attack. It is a rare condition.
Treatment of migraine: It includes home remedies, lifestyle modifications, medications and devices.
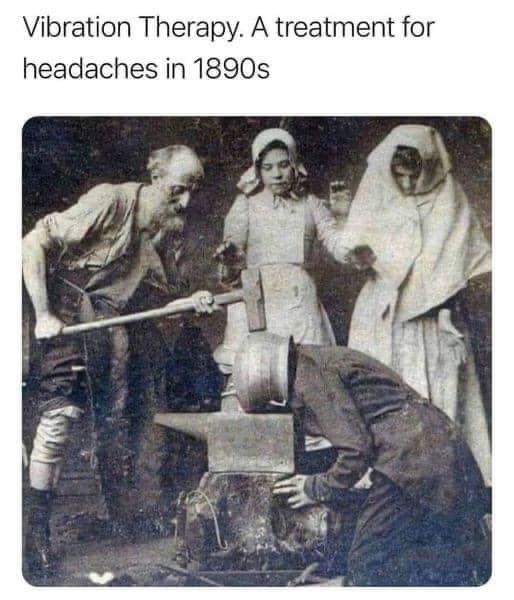 We are so fortunate that we do not live in 18th century!😃😃😃😃
We are so fortunate that we do not live in 18th century!😃😃😃😃
Home remedies include:
- Resting in a dark, quiet, cool room.
- Applying a cold compress or washcloth to your forehead or behind your neck. (Some people prefer heat.)
- Massaging your scalp.
- Yoga.
- Applying pressure to your temples in a circular motion.
- Keeping yourself in a calm state. Meditation helps.
Lifestyle modifications: These can be a large part of successful migraine prevention. Below is a list of proven strategies:
- Sleep: Maintain consistent sleep patterns, including on weekends and holidays. Learn how much sleep you need and try not to get too much or too little. Not getting enough sleep during the week and trying to get extra sleep on the weekend may trigger an attack. For more information, click here (SHHH…My Brain Is Sleeping)
- Exercise: A routine of 30 minutes of exercise 5 times per week can relieve stress and balance internal physiology. For more information: Dare to be Fit
- Eating: Eat regular meals, and do not skip meals. Eat a good, healthy breakfast. For more information: A Mindful Diet
- Reduce stress: Try some relaxation techniques, yoga, meditation etc. For more information: Brain Power Matters!
- Improve posture: Pay special attention to how you hold your neck and shoulders
- Stay hydrated: Dehydration can trigger the migraine. For more information: Are You Drinking Enough Water?
- Avoid overuse of painkillers: Such as Acetaminophen (Tylenol, Paracetamol), Ibuprofen, Aspirin or Naproxen (Aleve)
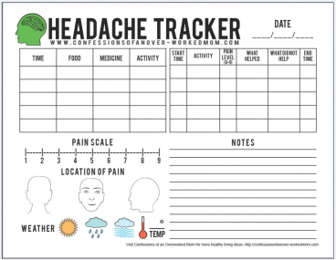
Headache diary or journal: Either you can use a paper-pencil or smartphone apps to note down the details about your migraine. Some important questions to answer in your migraine diary are:
- The date and time of when the migraine began
- What are your symptoms?
- How many hours of sleep you got the night before it happened?
- Is there any stress?
- Note the weather.
- Your food and water intake.
- Did you miss a meal?
- Describe the type of pain, its location, and its severity on a scale from 1-10 scale.
- Any pain medication you took.
- How long was the migraine?
- If you are a woman, are you on your period? etc.
The headache diary will help you to identify the triggers, and you can avoid them. This will be invaluable information for your doctor as it will help them accurately diagnose you and prescribe the best medication.
Drug therapy: There are two main treatment approaches that use medications: abortive therapy and preventive therapy
- Abortive therapy: Abortive medications or rescue medications are used to stop a migraine attack. These drugs work best if taken as soon as the attack begins. There are over-the-counter medicines like Acetaminophen (Tylenol, Paracetamol), Ibuprofen, Aspirin or Naproxen (Aleve). They are more effective when used in proper dose (under dosing or over dosing is not good) and also to be taken within 20-30 minutes after the onset of migraine. Overuse of these pain killers (using more than 2-3 times per week) can cause rebound headaches. So, be cautious! There are some abortive prescription medications like Triptans are available. Triptans are available in oral, nasal spray, injectable, transcutaneous patches.
- Preventive therapy: If you are experiencing at least four migraine attacks in a month and they are interfering with your daily activities, you might need preventive or prophylactic medication. These medications should be taken on a daily basis. There are different categories of these medications:
- Beta-blockers (Propranolol, Atenolol, Nadolol)
- Calcium channel blockers (Verapamil)
- Anti-seizure medications (Topiramate, Valproic acid)
- Antidepressants (Amitriptyline, Nortriptyline)
- Sometimes, a steroid is used.
- Calcitonin gene-related (CGRP) monoclonal antibodies (Erenumab(Aimovig), Fremanezumab, Galcanezumab)
Vitamins, minerals, herbs (Riboflavin/vitamin B2, Magnesium, Feverfew, Co-enzyme Q10) have been promoted as having efficacy (being helpful) for migraine prophylaxis (prevention).
Other: biofeedback therapy (a technique where people learn to sense changes in the body’s activity and to use relaxation and other methods to control the body’s responses), Acupuncture/Acupressure (fine metal needles or mechanical pressure are used to help the individual return to a balanced state), massage (relaxes the body, releases stress buildup in muscle tissue, and teaches body awareness) and Botox injections (used in chronic migraines).
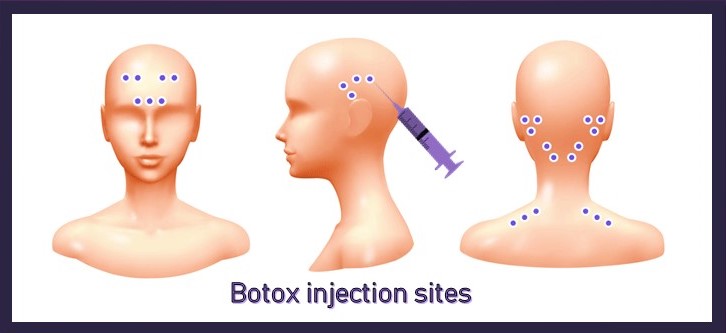
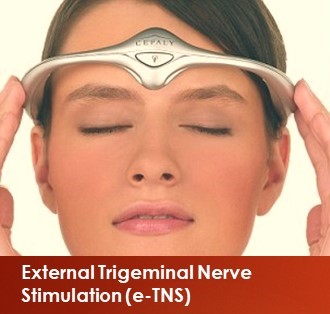
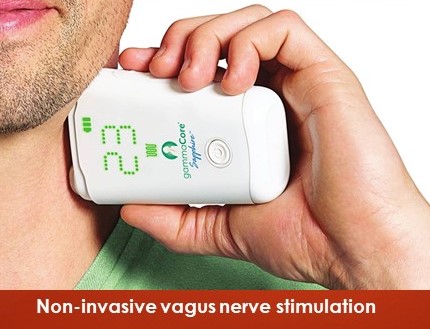
Migraine devices: The functional modification of neural circuits with electromagnetic current, delivered noninvasively via devices to treat migraine. It is called Neuromodulation. There are 3 FDA approved devices in USA. These devices use different approaches to affecting neuronal activity and are known as External Trigeminal Nerve Stimulation (e-TNS), Single Pulse Transcranial Magnetic Stimulator (sTMS), and non-invasive vagus nerve stimulation (gammaCore Non-Invasive Vagus Nerve Stimulator).

June is the migraine awareness month!

Great article savi! Not everybody know it’s a medical disabling condition!
Perfectly written! Keep it up!
Thank you!
Hi Savi,very informative article .
Thank you!
Nice article.
Nice article. For some it is a real handicap , effects work and relations
Yes, it can be a highly disabling condition. Thank you!
Very informative and nicely explained, thanks aunty & keep it up..👍👍
Thank you!
Very complex problem explained in very simple way 🙏
Thank you!
Very Informative and helpful article on Migraine.
Migraine sounds very common yet it is not as simple as we think if we leave it unaddressed.., and this article helps many out there to overcome this issue.
Thanks!
Thank you, Ramprasad. I am wondering what do you think of the title picture (model) 😉
Excellent article and very well written and useful for both doctors and patients
Thank you Dr Savitra, I will share with my son who suffers from severe migraine
You are a champ
Thank you, doctor!
Dr. Savitra, nice pictures! Can I use some of your pictures with reference to your website for my youtube videos?
Sure. Share your youtube link with me. Thanks
Hi Dr Savitra,
Your article is very informative. I was just wondering if you could throw some light on Vestibular migraine and how to handle these.
Thanks
Thank you, Aparna. The management of vestibular migraine is the same as for other types of migraines. Hope, it helps.