Click here to read the Marathi article: गियान बारे सिन्ड्रोम (जीबीयस) काय आहे?
Guillain-Barré Syndrome (GBS) is a rare but serious neurologic disorder. Raising awareness about GBS is important for early detection, timely treatment, and improving outcomes for those affected. It is being proposed that, Franklin D. Roosevelt, the 32nd president of the United States died at the age of 39 years due to GBS and not due to polio.
What is Guillain-Barré Syndrome?
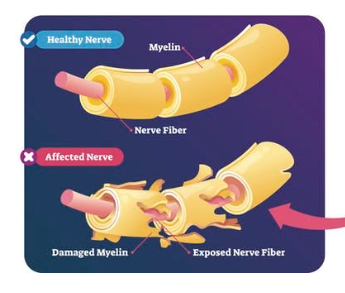
Guillain-Barré Syndrome is an autoimmune disorder where the body’s immune system mistakenly attacks the peripheral nervous system (which is the network of nerves outside the brain and spinal cord). It damages the myelin sheath, which is the protective covering of the nerves and disrupts the communication between the brain and the body. This damage often results in symptoms such as tingling sensations, muscle weakness, and even paralysis. In severe cases, GBS can cause respiratory failure, requiring mechanical ventilation.
GBS affects both adults and children, but in India, it has been observed more frequently in young adults and older children. It is not hereditary but is often triggered by infections such as:
- Campylobacter jejuni (a bacterial cause of diarrhea),
- Viruses like cytomegalovirus (CMV),
- Epstein-Barr virus (EBV),
- Zika virus,
- COVID-19.
- Dengue virus, Chikungunya in India
Rarely, it may also occur after vaccinations or surgeries. GBS is not contagious and is not caused by the infection itself, but rather by the immune system’s abnormal response to it.
How common is GBS?
- 1-2 cases per 100,000 people per year is the global average.
- In India, similar or slightly higher incidence, particularly where infections like Campylobacter jejuni, dengue, and other viruses are more common.
Symptoms and Progression:
GBS typically begins with weakness or tingling in the legs that can spread to the upper body and arms. Other symptoms include:
- Difficulty with facial movements (e.g., speaking, chewing)
- Loss of bladder control or bowel function
- Severe pain in certain areas like the shoulders and thighs
- Difficulty walking or climbing stairs
- Fluctuations in heart rate and blood pressure
- Difficulty breathing or swallowing (in severe cases)
Symptoms usually peak within two to four weeks before entering a plateau phase. Recovery may take weeks to months, with some individuals experiencing long-term effects such as residual weakness.
Diagnosis and Treatment:
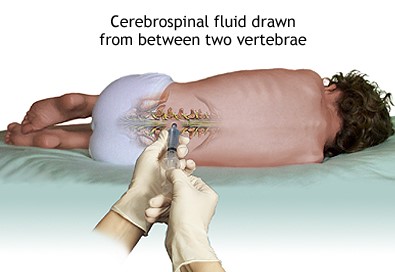
Diagnosing GBS involves a combination of medical history review, physical examinations, and tests such as lumbar punctures (to analyze brain/cerebrospinal fluid), electromyography (EMG), and nerve conduction studies. There is no specific blood test for GBS.

While there is no cure for GBS, treatments can reduce its severity and accelerate recovery. Common interventions include:
- Plasma Exchange (Plasmapheresis): Removes harmful antibodies from the bloodstream.
- Intravenous Immunoglobulin Therapy (IVIg): Uses healthy antibodies to block the harmful ones.
- Supportive Care: Includes respiratory support, physical therapy, and pain management during recovery.
Recovery: Recovery from GBS varies from person to person. Many regain full functionality with time and rehabilitation, while others may face lingering challenges.
Stages of Recovery:
- Acute Phase (0–4 weeks): This is when symptoms are progressing. Patients may experience increasing weakness, paralysis, or even require a ventilator to assist with breathing. Immediate treatment (such as IVIG or plasma exchange) is usually administered during this time.
- Plateau Phase (a few days to several weeks): Symptoms stop worsening but don’t improve much yet. The body begins to stabilize.
- Recovery Phase (months to years):Gradual healing begins. Nerves start to regenerate, and muscle strength and coordination return. This can be a slow process, and physical rehabilitation plays a major role.
- 80% of people are able to walk independently within 6 months.
- 60% fully recover motor strength within a year.
- A smaller group (around 15-20%) may have lasting weakness, fatigue, or pain.
- About 5% of cases may be fatal, usually due to complications during the acute stage.
How to prevent GBS?
Prevention is challenging because its exact cause remains unknown. It is often triggered by infections or other medical events. Hence, certain steps can help reduce the risk of developing GBS:
1. Avoiding Common Triggers
- Prevent infections: Since GBS is frequently triggered by bacterial or viral infections like Campylobacter jejuni, cytomegalovirus (CMV), Epstein-Barr virus (EBV), Zika virus, and influenza, maintaining good hygiene practices such as washing hands regularly and cooking food thoroughly (especially poultry) can reduce exposure to these pathogens.
- Vaccination awareness: While vaccines rarely trigger GBS, staying informed about vaccine-related risks and discussing concerns with a healthcare provider can help make informed decisions.
2. Managing Health Conditions
- Strengthen immunity: A healthy lifestyle, including a balanced diet, regular exercise, and adequate sleep, can support the immune system and lower the risk of abnormal immune responses. Click here to know more about immunity: ‘I’ For Immunity
Take home points:
- Guillain-Barré Syndrome is a complex condition that requires greater social awareness to ensure early diagnosis and effective treatment.
- By educating communities about its symptoms, triggers, and management options, we can support those affected by this condition while fostering research into better therapies.
- Knowledge about GBS not only empowers individuals but also strengthens public health responses to neurological disorders worldwide.
- Prevent infections by adopting good hygiene practices, and strengthen your immunity.
- Let us work together to spread awareness and provide hope for those battling Guillain-Barré Syndrome.
Vast but minute information about GBS . Non medico also know GBS frm ur information. Good one savi. Keep it up.