
When we eat food, it gets digested in the stomach. Many foods, mainly carbohydrates, break down into glucose. Blood glucose is the main source of energy for our brain, heart and muscles. Blood sugar either comes from the food we eat or is made by the liver. It is found in the blood stream (as it is carried to all of our organs and cells) and inside the cells (where it is changed into energy). The pancreas is a gland, located just behind the stomach. It is about the size of a hand. Pancreas secretes a hormone called as insulin. When insulin is released from the pancreas, it travels through the bloodstream to the body’s cells and tells the cell doors to open up to let the glucose in. Then the cells convert glucose into energy to use or store it to use later. As glucose moves from the blood into the cells, blood sugar levels start to drop. The pancreas slows down making insulin. The rise and fall in insulin and blood sugar happens many times during the day and night.
What is Diabetes?
Diabetes mellitus, commonly known as diabetes, is a disease that occurs when your blood glucose (sugar) is too high. With diabetes, your body either doesn’t make enough insulin or can’t effectively use the insulin it does make. Glucose cannot enter the cells where it is needed. So, the amount of glucose in the blood continues to rise. This is called hyperglycemia (high blood sugar).
When the body does not have enough insulin to help convert sugar into energy, it starts burning body fat instead. But burning too much fat for energy produces a byproduct called ketones. High levels of ketones can lead to a condition called diabetic ketoacidosis (DKA), which can be life threatening (diabetic coma and death) if not treated quickly. DKA usually occurs in diabetes type 1.
There are few types of diabetes:
Prediabetes occurs when your blood sugar is higher than normal, but it is not high enough for a diagnosis of type 2 diabetes.
Type 1 diabetes is an autoimmune disease. The immune system attacks and destroys cells in the pancreas, where insulin is made. It is unclear what causes this attack. About 10 percent of people with diabetes have this type. It often starts in childhood.
Type 2 diabetes occurs when your body becomes resistant to insulin, and sugar builds up in your blood. It accounts for >90 percent of diabetes in adults. It was so rare in children before. Now that more children are overweight or obese, type 2 diabetes is becoming more common in this age group.
Gestational diabetes is high blood sugar during pregnancy. Insulin-blocking hormones produced by the placenta cause this type of diabetes.
Diabetes is one of the fastest growing health challenges of the 21st century, with the number of adults living with diabetes having more than tripled over the past 20 years. The incidence of diabetes is 9.4% in USA and 11.8% in India. The continued rise is largely due to environmental, genetic factors, changing lifestyle habits (e.g. higher calorie intake, increasing consumption of processed foods, sedentary lifestyles leading to obesity) and urbanization.
Your chances of developing type 2 diabetes depend on a combination of risk factors such as your genes and lifestyle. Although you cannot change risk factors such as family history, age, or ethnicity, you can change lifestyle risk factors around eating, physical activity, and weight. These lifestyle changes can affect your chances of developing type 2 diabetes.

Risk factors for diabetes type 2: if you
- Are overweight or obese
- Age 45 or older
- Have a family history of diabetes
- Are African American, Alaska Native, American Indian, Asian American, Hispanic/Latino, Native Hawaiian, or Pacific Islander
- Have high blood pressure
- Have a low level of HDL (“good”) cholesterol, or a high level of triglycerides
- Have a history of gestational diabetes or gave birth to a baby weighing 9 pounds (>4 Kg) or more
- Are not physically active
- Have a history of heart disease or stroke
- Have depression
- Have polycystic ovary syndrome, also called PCOS
- Have acanthosis nigricans—dark, thick, and velvety skin around your neck or armpits
Sometimes certain medicines can harm beta cells of pancreas which secrete insulin. These include
- Niacin, a type of vitamin B3
- Certain types of diuretics, also called water pills
- Anti-seizure drugs
- Psychiatric drugs
- Drugs to treat human immunodeficiency virus (HIV)
- Pentamidine, a drug used to treat a type of pneumonia
- Glucocorticoids—medicines used to treat inflammatory illnesses such as rheumatoid arthritis, asthma, lupus and ulcerative colitis
- Statins, which are medicines to reduce LDL (“bad”) cholesterol levels, can slightly increase the chance of diabetes
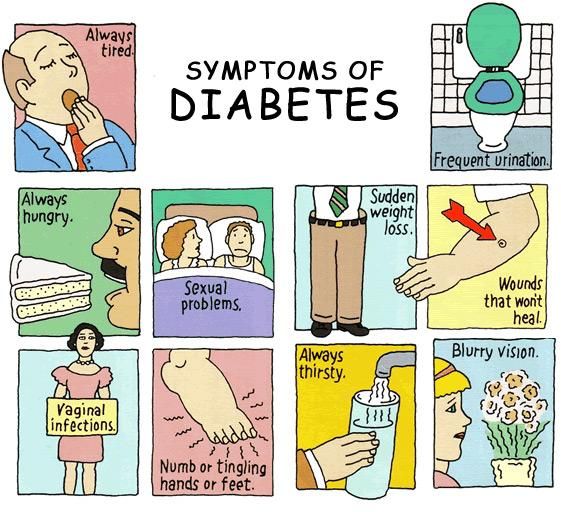
Symptoms of type 1 diabetes can start quickly, in a matter of weeks. Symptoms of type 2 diabetes often develop slowly—over the course of several years—and can be so mild that you might not even notice them. Many people with type 2 diabetes have no symptoms. Some people do not find out they have the disease until they have diabetes-related health problems, such as blurred vision or heart trouble.
Symptoms of diabetes include
- Increased thirst and urination
- Increased hunger
- Fatigue
- Blurred vision
- Numbness or tingling in the feet or hands
- Sores that do not heal
- Unexplained weight loss
 The American Diabetes Association recommends screening for type 2 diabetes in
The American Diabetes Association recommends screening for type 2 diabetes in
- Age 45 or older (get tested every year)
- Between the ages of 19 and 44 who are overweight (BMI≥25)
- 1st degree relative with diabetes
- Physically inactive
- Hypertension (>140/90) or taking medication for hypertension
- PCOS (polycystic ovary syndrome)
- Plasma high-density lipoprotein cholesterol level <35 mg/dl or triglyceride level >250 mg/dl
- History of CVD (Cardiovascular disease)
- History of gestational diabetes mellitus or delivery of a baby weighing > 9 lb (4.1 kg)
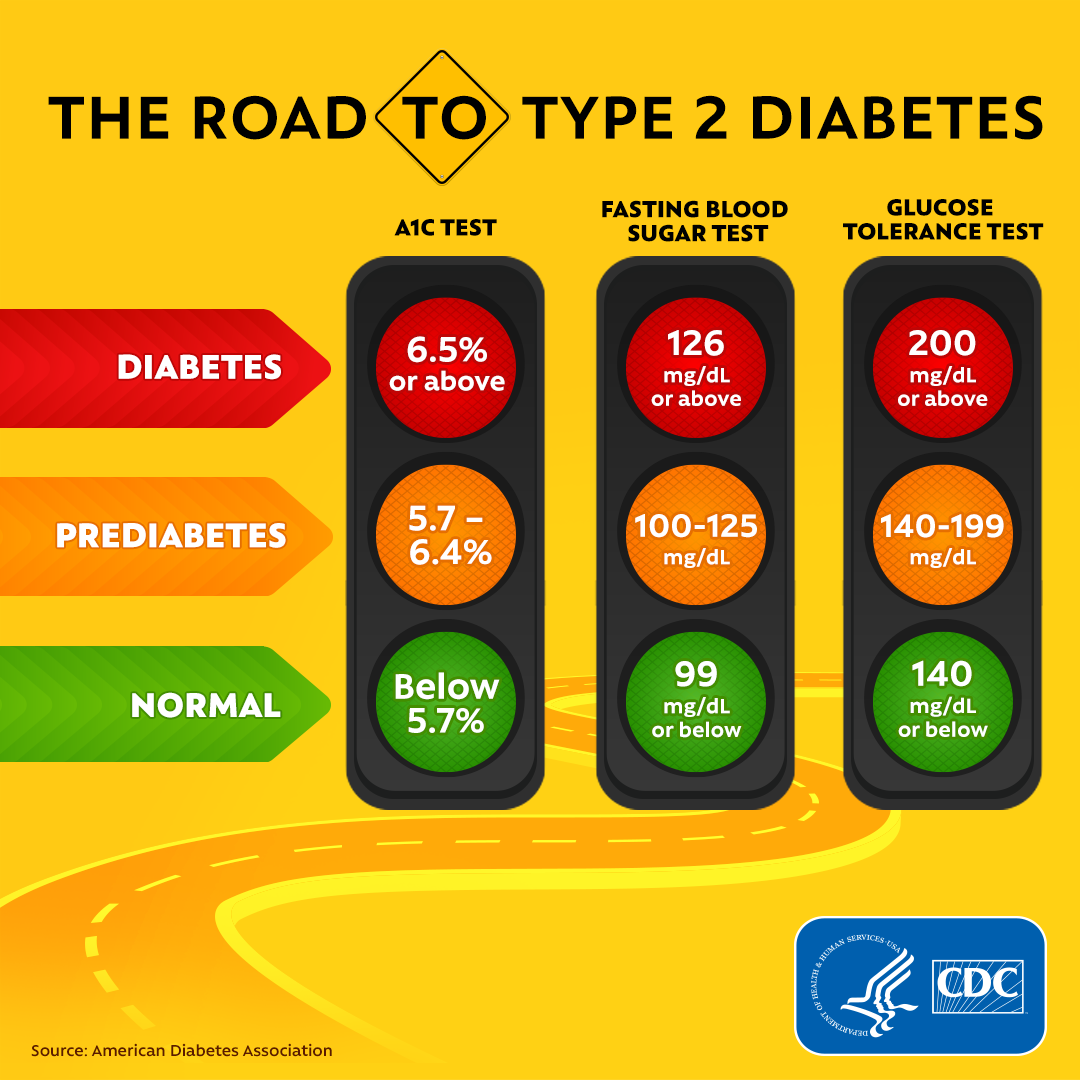
The diagnosis can be made with:
- A fasting plasma glucose (FPG) level of 126 mg/dL or greater: measures your blood glucose level at a single point in time. For the most reliable results, it is best to have this test in the morning, after you fast for at least 8 hours. Fasting means having nothing to eat or drink except sips of water.
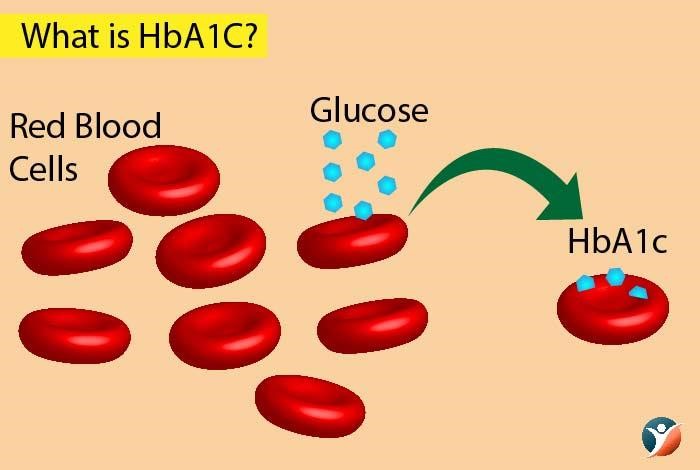
- An HbA1C level of 6.5% or greater: provides your average levels of blood glucose over the past 3 months. Other names for the A1C test are hemoglobin A1C, HbA1C, glycated hemoglobin, and glycosylated hemoglobin test. Hemoglobin is a protein found in red blood cells. It gives blood its red color, and its job is to carry oxygen throughout your body. When glucose builds up in your blood, it binds to the hemoglobin in your red blood cells. The A1c test measures how much glucose is bound. Red blood cells live for about 3 months, so the test shows the average level of glucose in your blood for the past 3 months. You can eat and drink before this test. The higher the percentage, the higher your average blood glucose levels.

- A random plasma glucose (RPG) level of 200 mg/dL or greater: RPG test is to diagnose diabetes when diabetes symptoms are present. You do not need to fast overnight for the RPG test. You may have this blood test at any time.
I am diagnosed with diabetes Type 2! Now what?
Although diabetes has no cure, you can take steps to manage your diabetes and stay healthy. Diagnosis of type 2 diabetes is often a powerful motivator for lifestyle change.
This article is mainly focused on diabetes Type 2 and following aspects are covered in it:
- Weight management
- Diabetes meal planning (separate article on it)
- Physical activity
- Medicines to control blood sugar levels
- Mental health in diabetes
- Prevent complications
- Heart disease
- Stroke
- Kidney disease
- Nerve damage
- Sexual problems
- Urinary tract infections
- Foot health
- Oral health
- Hearing loss
- Vision loss
- Vitamin D and diabetes
- Vitamin B12 supplementation
1. Weight management:
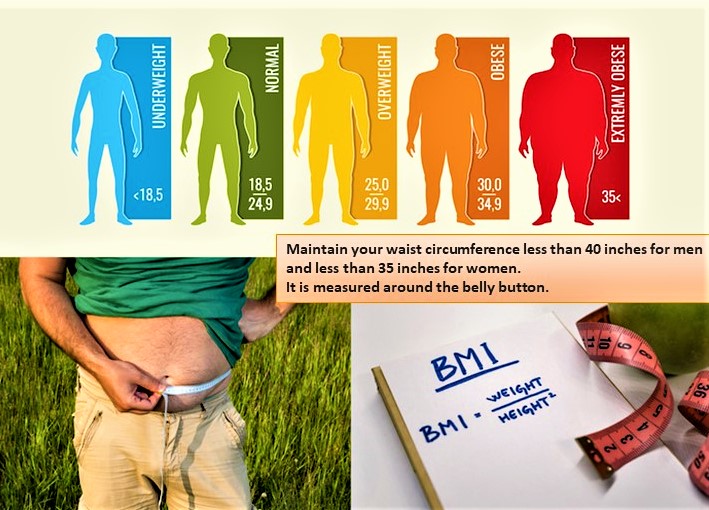
Weight management: we learned that insulin resistance is a major risk factor for type 2 diabetes. People who are overweight, especially if they have excess belly fat, are more likely to have insulin resistance and eventually diabetes. Due to growing problem of overweight/obesity in children, type 2 diabetes is seen in some as young as 10 years old. Try to keep your BMI 18.5 to 25 kg/m2. You can calculate your BMI here: Adult BMI Calculator
2. Diabetes Meal Planning: I wrote another article with the guidelines to help to make your diabetes meal plan. Click here: Diabetes Meal Planning
3. Physical activities:
Exercise improves blood glucose control in type 2 diabetes by making your body more sensitive to insulin. It reduces cardiovascular risk factors and lowers the risk of nerve damage. Some additional benefits include:
- Maintaining a healthy weight
- Losing weight, if needed
- Feeling happier
- Sleeping better
- Improving your memory
- Controlling your blood pressure
- Lowering LDL (“bad”) cholesterol and raising HDL (“good”) cholesterol
The goal is to get at least 150 minutes per week of moderate-intensity physical activity. One way to do this is to try to fit in 30 minutes of activity for 5 times a week.
Examples of moderate-intensity physical activities include:
- Walking briskly
- Doing housework
- Mowing the lawn
- Dancing
- Swimming
- Bicycling
- Playing Sports
Include aerobic exercise, muscle strengthening and stretching exercise. For more information, click here: Dare to be fit!
- Drink plenty of fluids while being physically active to prevent dehydration. For more information, click here: Are You Drinking Enough Water?
- Make sure to check your blood sugar before being physically active, especially if you take insulin.
- Wear cotton socks and athletic shoes that fit well and are comfortable.
- After being physically active, check your feet for sores, blisters, irritation, cuts, or other injuries.
Physical activities can lower your blood sugar level. Low blood sugar (hypoglycemia) is defined as a blood sugar level below 70 milligrams per deciliter (mg/dL).
Pay attention to the early warning signs of hypoglycemia, and treat low blood sugar promptly. You can raise your blood sugar quickly by eating or drinking a simple sugar source, such as glucose tablets or fruit juice. Tell family and friends what symptoms to look for and what to do if you’re not able to treat the condition yourself. If untreated, hypoglycemia can lead to: Seizures, loss of consciousness and death ☹
Also, when blood sugar goes >200, it is called hyperglycemia. Hypoglycemia is more dangerous than hyperglycemia.

4. Medicines to control blood sugar levels:
Some people with type 2 diabetes can manage their disease by making healthy food choices and being more physically active. Many people with type 2 diabetes need diabetes medicines as well. In certain conditions, they might have to use Insulin. These medicines may include diabetes pills (Metformin, Glyburide, Glimepiride, Glipizide, Nateglinide, Rosiglitazone, Acarbose, Sitagliptin etc) or insulin (injections or shots; insulin pen, insulin pump, inhaler or jet injector). Oral diabetes medications may also come in combination tablets.
5. Mental health in diabetes:
Diabetes Distress: You may sometimes feel discouraged, worried, frustrated, or tired of dealing with daily diabetes care. This overwhelming feeling is known as diabetes distress. You might feel that diabetes is controlling you instead of you controlling it. You might experience it when you do not see the good results or you have developed a diabetic complication in spite of working hard. There is no medicine for it. Consider seeing a mental health counselor. People with diabetes are 2 to 3 times more likely to have depression than people without diabetes. If you are stressed, stress hormones make blood sugar rise or fall unpredictably. Being stressed for a long time can lead to other health problems or make them worse. Risk of anxiety is 20% more in people with diabetes than normal people. The earlier you get treated for anxiety or depression, better your quality of life and your diabetes. You might need medicines, therapy or both. Adopt a healthy lifestyle by being physically active, getting enough sleep, doing some relaxation exercises like meditation or yoga. For more information, click here: Brain Power Matters!
6. Prevent complications of diabetes:
Heart disease: Heart disease is the leading cause of death among people with diabetes. Over time, high blood sugar from diabetes can damage blood vessels as well as the nerves that control your heart and blood vessels. Follow a healthy diet, aim for a healthy weight, get physically active, get a regular HbA1C test, keep your blood pressure below 140/90 mm Hg, control your cholesterol levels and stop smoking. Your doctor might recommend Aspirin based on clinical judgement. A heart attack usually occurs when a blood clot blocks blood flow to the heart. Symptoms include tightness or pain in the chest, neck, back, or arms, as well as fatigue, lightheadedness, abnormal heartbeat, and anxiety. Diabetes can cause a silent heart attack, means it could happen without you even knowing it or it could feel like heartburn. It is due to neuropathy (nerve damage) affecting nerves of your heart.
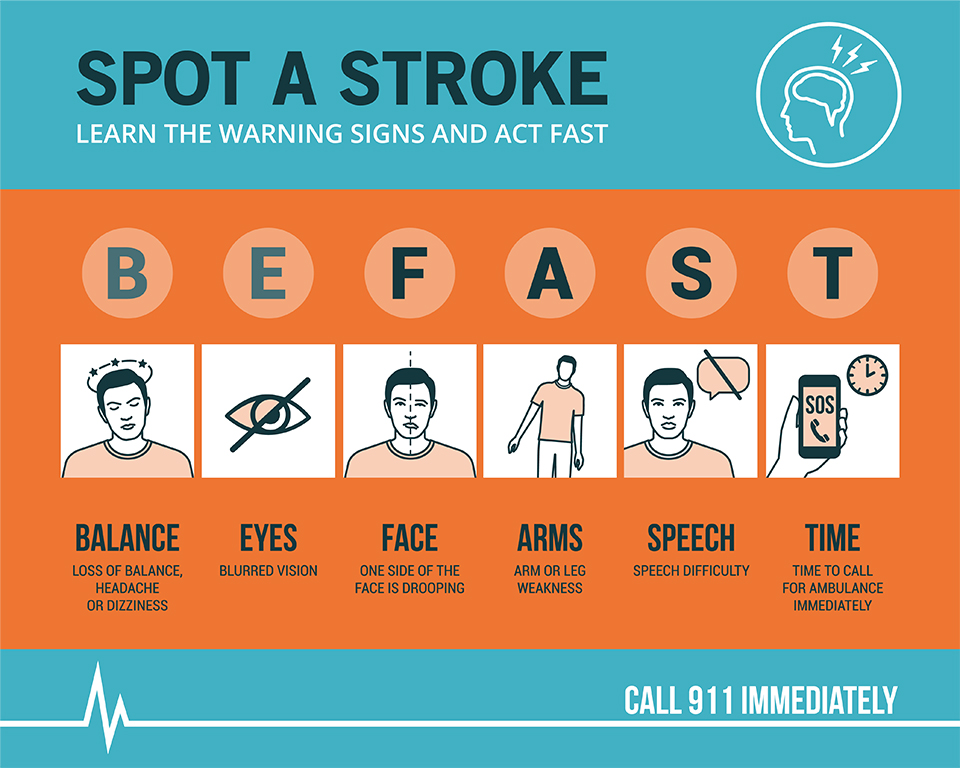
Stroke: A stroke happens when the blood supply to part of your brain is suddenly interrupted. Then brain tissue is damaged. Most strokes happen because a blood clot blocks a blood vessel in the brain or neck. If you have diabetes, your chances of having a stroke are 1.5 times higher than in people who don’t have diabetes.
Kidney disease: High blood sugar damages cells and blood vessels in your kidneys so they can’t filter out waste as well as they should. This condition is called chronic kidney disease, or CKD. About 1 in 3 adults with diabetes has CKD. Stay in your target blood sugar range as much as possible, and keep your blood pressure below 140/90 mm Hg. CKD doesn’t have any signs or symptoms at first, so it’s important to get your kidneys checked regularly by checking GFR and albuminuria. GFR (glomerular filtration rate), a blood test that checks how well your kidneys are filtering your blood. Albumin is a protein that can pass into the urine when the kidneys are damaged. It can be tested by a urine test to check for albumin.
Nerve damage: Over time, high blood sugar can cause neuropathy (nerve damage) throughout your body. One type of neuropathy affects the nerves in your arms and legs. Symptoms can range from mild numbness to pain that makes it hard to do normal activities. The other type of neuropathy can affect your heart, stomach, and other organs in your body. As many as half of people with diabetes have nerve problems, but not all have symptoms. The longer you have diabetes, the more likely you’ll have nerve damage. Gastroparesis is a condition where the stomach doesn’t empty normally because of nerve damage. This can cause your blood sugar to rise when food finally leaves your stomach. Your blood sugar levels can be hard to predict and make your diabetes harder to manage. Symptoms of gastroparesis can include heartburn, nausea, vomiting, feeling full quickly, weight loss, loss of appetite, and abdominal bloating.

Sexual problems: Many people with nerve damage from diabetes have trouble having sex. Men can have trouble maintaining an erection and ejaculating; and women can have trouble with arousal and vaginal lubrication.
Urinary tract infections: Both men and women with diabetes are more likely to get urinary tract infections and have bladder problems.
Foot health: Nerve damage can lower your ability to feel pain, heat, or cold. If you don’t feel pain in your feet, you may not notice a cut, blister, or sore, or that water is too hot. Small problems can become serious if they aren’t treated early. Poor circulation (another diabetes complication) along with nerve damage puts you at risk for developing a foot ulcer (a sore or wound) that could get infected and not heal well. If an infection doesn’t get better with treatment, your toe, foot, or part of your leg may need to be amputated (removed by surgery) to prevent the infection from spreading.
What are some ways I can take care of my feet?
- Check your feet every day for cuts, redness, swelling, sores, corns, calluses, or blisters.
- Wash your feet in warm—not hot—water, and dry them well.
- Trim your toenails straight across and file the edges with an emery board.
- Wear shoes that fit well. Break in new shoes slowly by wearing them 1 to 2 hours each day until they’re comfortable.
- Never go barefoot. Always wear shoes or slippers, even inside, to protect your feet.
- Put your feet up when you’re sitting and wiggle your toes for a few minutes.
- Get your feet checked at every health care visit, and see your foot doctor every year (more often if you have nerve damage).

Oral health: High blood sugar increases the level of sugar in your saliva. Sugar feeds the bacteria in your mouth, and when bacteria is combined with food, it creates plaque, a sticky film that can cause tooth decay. People with diabetes are more likely to have gum disease, which can lead to tooth loss. Gum disease can also make blood sugar levels rise and make diabetes harder to manage. Treating gum disease can lower blood sugar over time and reduce the chance of other diabetes problems, such as heart disease and kidney failure. Brush your teeth at least twice a day and floss once a day. Get regular dental checkups, and let your dentist know you have diabetes.
Hearing loss: Hearing loss is twice as common in people who have diabetes compared to normal people. Over time, high blood sugar levels can damage small blood vessels and nerves in the inner ear. This may also affect your balance. Hearing loss often happens gradually, so you may not know you’re having trouble hearing.
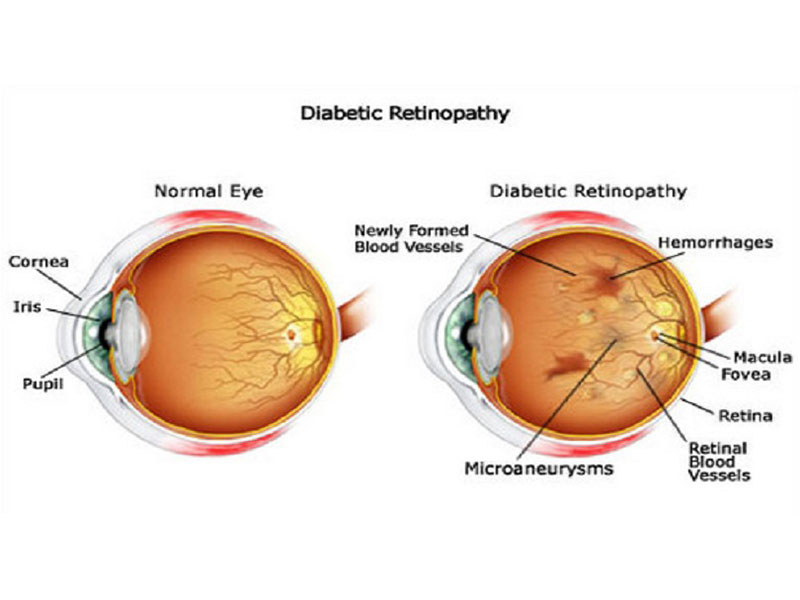
Vision loss: Diabetic retinopathy is a very common diabetes complication, and it’s the leading cause of blindness. High blood sugar levels and high blood pressure can damage small blood vessels in the retina (the light-sensitive layer at the back of the eyeball). Usually both eyes are affected. People with diabetes are also more likely to develop cataracts (clouding of the lens) and glaucoma (a group of diseases that damage the optic nerve). You may not even have any symptoms until you start to lose your vision, so regular eye exams are necessary. Visit your eye doctor for a dilated eye exam at least once a year.
7. Vitamin D and diabetes:
There is growing evidence that vitamin D deficiency could be a contributing factor in the development of both type 1 and type 2 diabetes. Some studies support the notion that adequate vitamin D supplementation may decrease the incidence of type 1 and possibly also of type 2 diabetes mellitus and may improve the metabolic control in the diabetes state. However, the exact mechanisms are not clear and need further investigation. Read more about Vitamin D at: Vitamins and Minerals.
8. Vitamin B12 supplementation:
Vegetarian diets are low in vitamin B12. Vitamin B12 is needed to maintain the health of nerve fibers. Low levels can cause tingling and numbness in the hands and feet (sometimes called glove and stocking anesthesia). Metformin is the recommended and most effective first-line drug for type-2 diabetes but its use has also been linked to vitamin B12 deficiency, which increases the risk of peripheral nerve damage. Check your Vitamin B12 level and use supplements as per your doctor’s instructions. Read more about Vitamin B12 at: Vitamins and Minerals.
Your diabetes care schedule:
- Check your blood sugar level several times a day as directed by your doctor. Keep a record of your numbers and share with your health care team during your next visit.
- Do HbA1C test every 3 months.
- Get dental exam every 6 months.
- Complete foot check, kidney tests (GFR, urine albumin test). Dilated eye exam and cholesterol test every year.
- Stay healthy and be happy!
References:
- https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes
- https://www.diabetes.org/diabetes
- https://www.cdc.gov/diabetes/managing/eat-well/meal-plan-method.html
- https://medlineplus.gov/ency/patientinstructions/000941.htm
- 7-day-indian-diet-plan-for-type-2-diabetes
Very nice article, thoroughly covered all aspects,of the diabetes and its occurence, complications and management.Specialy how to take care,screening,dietery planning,drugs management.
Thank you for taking time to give me feedback!
Very informative article. Thank you very much for sharing.
Thank you.
Thank you, this is very informative 👍🏻👍🏻
Thank you for sharing this valuable info. Very informative and useful. 👌👌🙏🏼