Pediatric neurologists (also known as child neurologists) are medical doctors who have completed four years of medical school, two years of residency training in Pediatrics, and three years of training in child neurology, which includes one year of training in adult neurology. Pediatric neurologists are board certified by the American Board of Psychiatry and Neurology (ABPN) with special qualifications in Child Neurology! 😎
The first board certification in Child neurology was awarded in 1968. At present, there are over 70 university-based training programs in child neurology in the United States and Canada.
Some child neurologists complete an additional 1-2 years of fellowship, where they learn a sub-specialty within neurology, such as epilepsy, neuromuscular diseases, stroke, neurophysiology, sleep medicine, pain medicine, sports medicine, headaches, oncology, neuroendocrinology, neurocritical or movement disorders.
Child neurologists often work closely with physical therapists, occupational therapists, speech therapists, psychologists, child psychiatrists and school guidance counselors to help your child develop and learn to the best of their potential.
They evaluate children with a wide range of developmental and neurological conditions including but not limited to:
Seizures and epilepsy: 40-50% of cases in pediatric neurology are epilepsy. A child may have one or more types of seizures (or convulsions), with symptoms causing changes in awareness, muscle tone, emotions, behavior and sensory experience.1 When child has a tendency to have recurrent seizures, it is called an epilepsy.
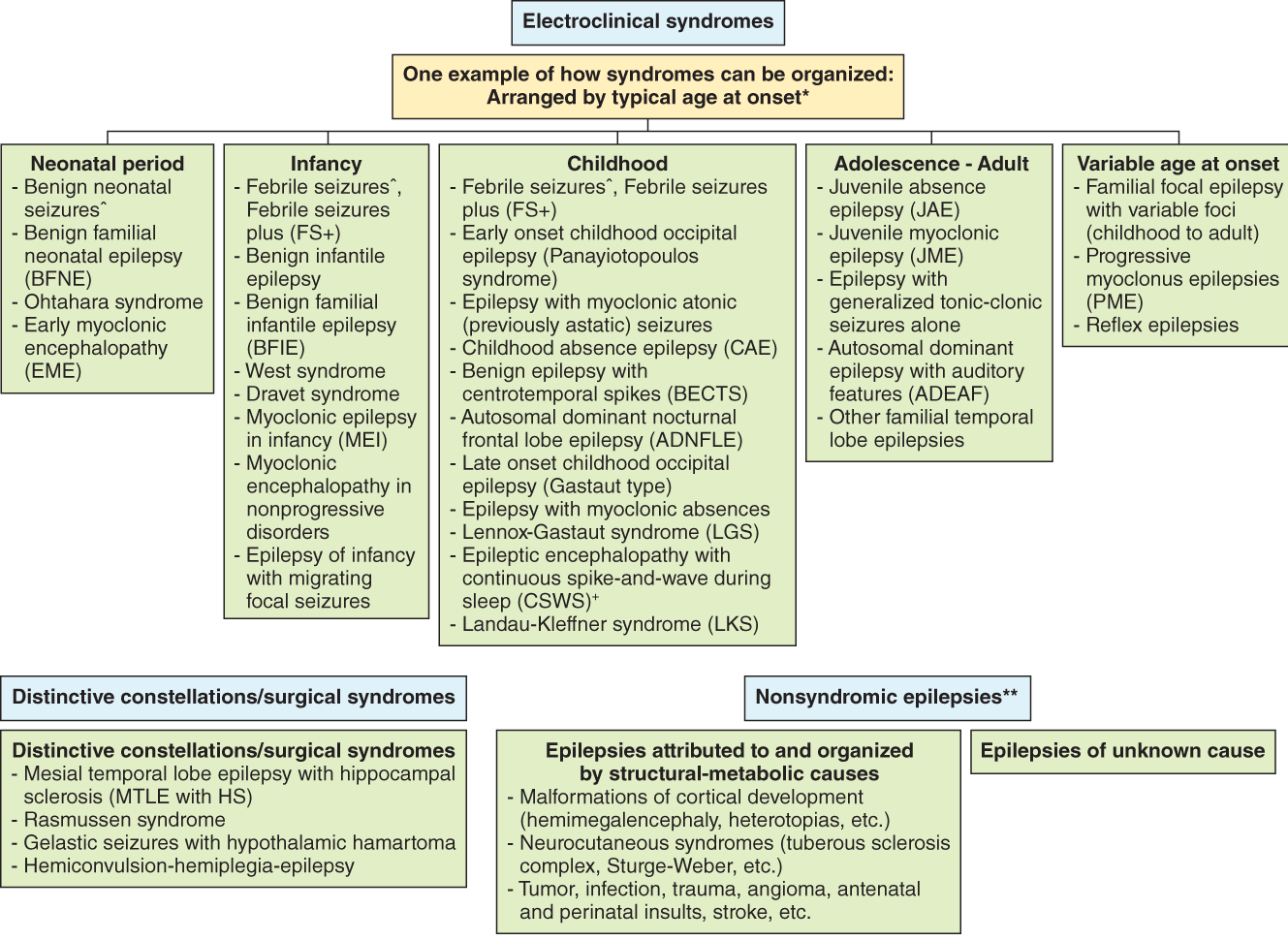
There are different types of seizures including, but not limited to, grand mal (whole body experiences shaking and the muscle stiffening), focal seizures (only one part of the body is involved), petit mal (staring into space), laughing seizures, myoclonic seizures (sudden muscle jerks), etc. The following table gives an idea of the numerous types of epilepsies:
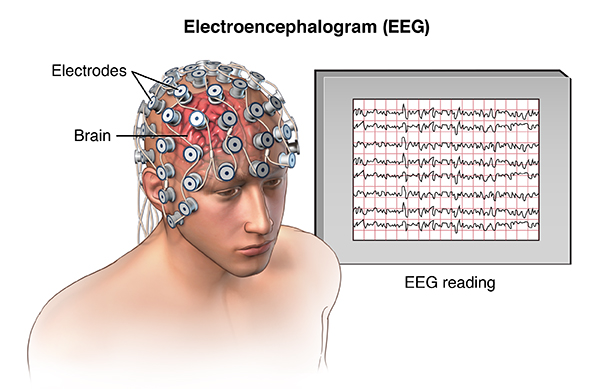
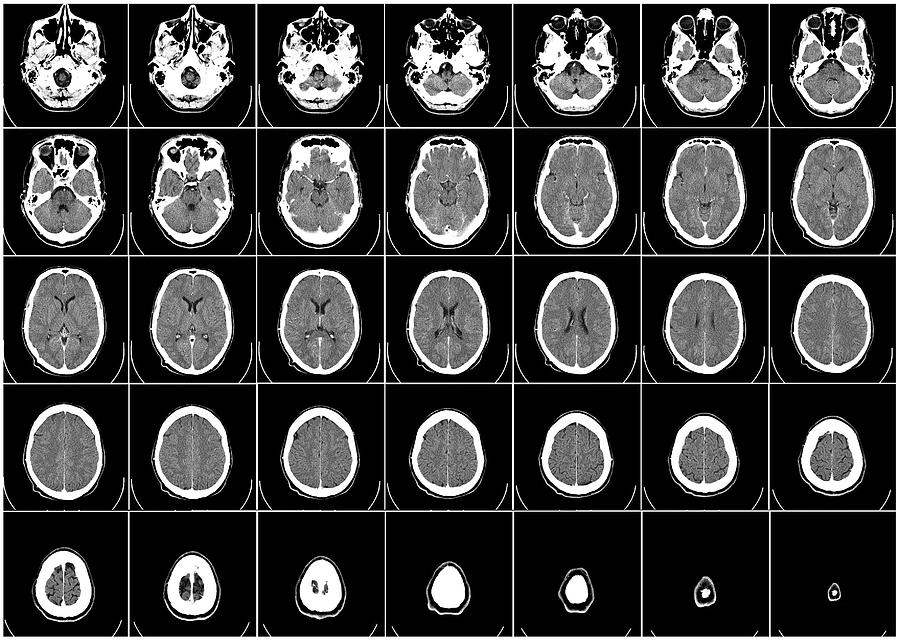
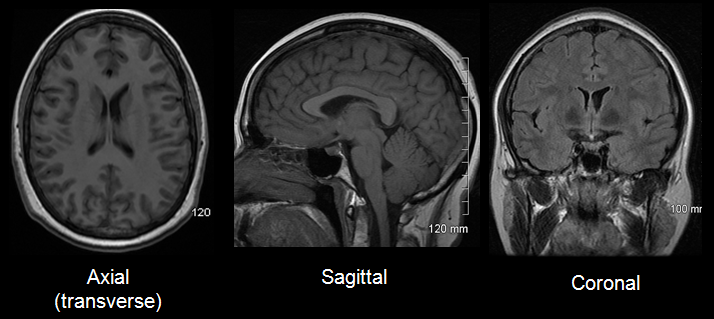
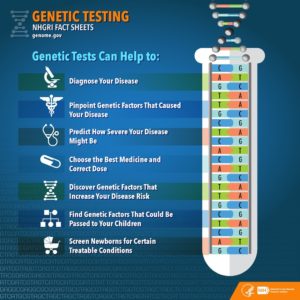
A child may have to go through some tests like electroencephalogram (EEG) which detects electrical activity in the brain, brain scan either computerized tomography (CT) or magnetic resonance imaging (MRI) which is an imaging technique to form brain pictures. In some cases, along with blood tests, genetic tests, cerebrospinal fluid (CSF, which is brain fluid) tests are necessary. Some conditions need anti-epileptic drug (AED) for some time or lifelong; whereas some conditions do not need any treatment. In some conditions, a specific diet known as ketogenic diet is used and some cases need surgery.
Febrile seizures: In the age group of 6 months to 5 years, some children get seizures or convulsions with fever from infection. Febrile seizures are more likely to occur if there is a family history of febrile seizures. The fever may accompany common childhood illnesses such as a cold, flu, or an ear infection. In some cases, a child may not have a fever at the time of the seizure but will develop one a few hours later2.
Most febrile seizures last only a few minutes and are accompanied by a fever above 101°F (38.3°C). Febrile seizures can be named as either simple febrile seizures or complex febrile seizures (=are febrile seizures that last longer than 15 minutes, more than one seizure in 24 hours, or seizures in which only one side of the body is affected). Although they can be frightening for parents, brief febrile seizures (less than 15 minutes) do not cause any long-term health problems.
Having a febrile seizure does not mean a child has epilepsy. But febrile seizures may carry an increased risk of developing epilepsy. Most children do not require daily treatment with medication. Febrile seizures cannot be controlled by controlling the fever. In case of prolonged febrile seizure, medication can be used which terminates the seizure. Simple febrile seizures usually do not require EEG and brain MRI.
Developmental Delays: including language, fine motor, or gross motor challenges. Children do not achieve age appropriate developmental milestones.


These children need neurological evaluation to check underlying cause(s) for the delay and eventually need therapies. Speech therapy for speech and language delay, physical therapy for gross motor delay and occupational therapy for fine motor delay. Sometimes, they need blood tests, brain/spine MRI, electroencephalogram (EEG) and genetic tests. They can have delays in cognitive skills and social emotional skills. If delay occurs in many or all of these areas, it is called as global developmental delay (GDD). If child is less than 3-year-old, he/she can get therapies through early intervention program (EIP) and therapists go to their house to provide therapies. Once child turns 3 and if he/she continues to need therapies, they can receive it at school through individualized education plan (IEP).
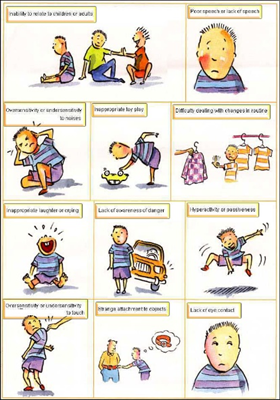
Autism Spectrum Disorder (ASD): ASD is a lifelong developmental disability that affects how people perceive the world and interact with others. They see, hear and feel the world differently to other people. The prevalence of ASD in the United States is about one in 54 children. More common in boys than girls. Children with ASD have social-communication problem, repetitive behaviors, rigid thinking, sensory processing issues (over- or under-sensitivity to sounds, touch, tastes, smells, light, colors, temperatures or pain). It is due to combination of factors – genetic and environmental. Autism is not caused by a person’s upbringing, their social circumstances and is not the fault of the individual with the condition.
There is no cure for it. Early identification and interventions with therapies may help reduce symptoms and build skills. Behavioral therapy, called as ABA (applied behavioral analysis) is the oldest and most fully researched treatment. It is diagnosed clinically as there is no test available for the diagnosis. The subtypes, Asperger syndrome, pervasive developmental disorders not otherwise specified (PDD-NOS) and autism are no longer used since 2013. If child meets diagnostic criteria on the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, 5th Edition) scale, he gets the diagnosis of ASD. No two children with ASD are same.
They can have different functional levels:
Level 1 (high functioning),
Level 2 (moderately severe), or
Level 3 (severe).
Vaccines do not cause autism!👈
Intellectual disability (ID):The old term mental retardation is replaced with ID. IQ (intelligence quotient) is measured by an IQ test. The average IQ is 100, with the majority of people scoring between 85 and 1153. A person is considered intellectually disabled if he or she has an IQ of less than 69. ID is characterized by below-average intelligence or mental ability and a lack of skills necessary for day-to-day living.
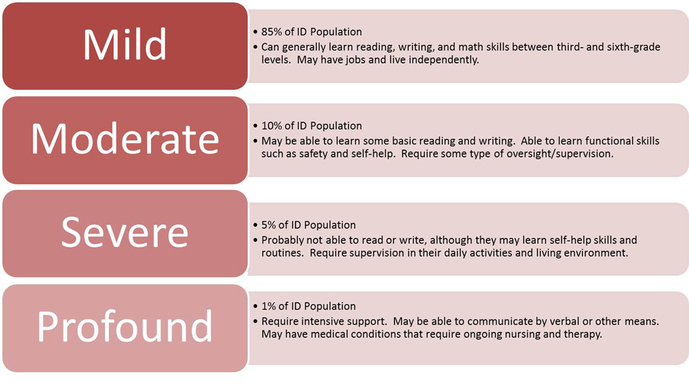
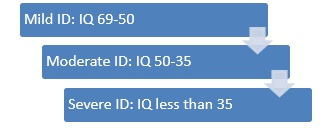 People with intellectual disabilities can and do learn new skills, but they learn them more slowly. There are varying degrees of intellectual disability, from mild to profound ID.
People with intellectual disabilities can and do learn new skills, but they learn them more slowly. There are varying degrees of intellectual disability, from mild to profound ID.
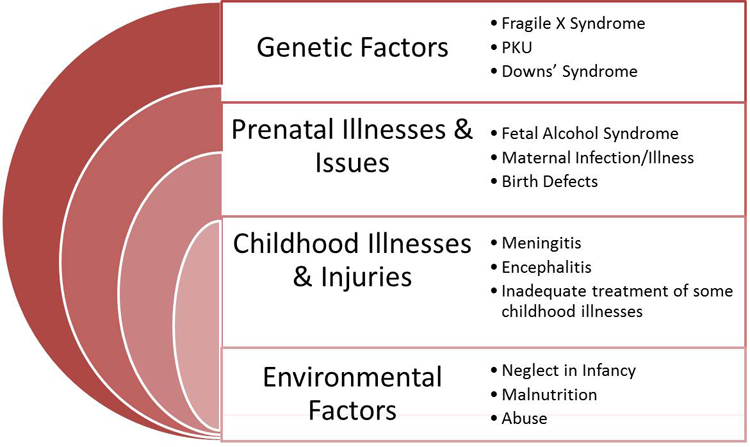
The common causes are genetic conditions (like Down syndrome, Fragile X syndrome), complications during pregnancy interfering with fetal brain development (like alcohol, drugs, infections, malnutrition and preeclampsia), problems during childbirth (oxygen deprivation, extremely premature baby), infections or injury after birth. But in some cases, cause is unknown.
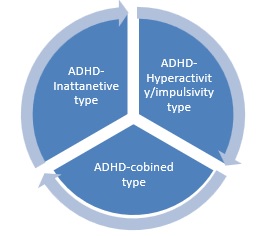
Attention Deficit Hyperactivity Disorder (ADHD):
It is a neurodevelopmental disorder affecting 11% of school-age children in US.4
Symptoms continue into adulthood in more than three-quarters of cases. ADHD is characterized by developmentally inappropriate levels of inattention, impulsivity and hyperactivity. The exact cause is unknown, but scientists have discovered a strong genetic link since ADHD runs in families. There are some environmental factors which can increase the likelihood of having ADHD like exposure to pesticides, premature birth, brain injury, fetal exposure to alcohol or drugs. ADHD is due to functional impairments in some brain’s chemical system, known as neurotransmitter system involving dopamine and norepinephrine. Depending on symptoms,
ADHD is typed into 3 subtypes:
Inattentive type (difficulty paying attention, poor organizing skills, very forgetful, gets easily distracted);
Hyperactivity/impulsivity type (unable to sit still, fidgets, very talkative, interrupts, unable to wait for his turn) and
Combined type when they have inattentive as well as hyperactivity/impulsivity symptoms together.
They can be very successful in life. However, without identification and proper treatment, ADHD may have serious consequences, including school failure, family stress and disruption, depression, problems with relationships, substance abuse, delinquency, accidental injuries and job failure. Early identification and treatment are extremely important.
There is no genetic test, blood test, EEG or neuroimaging to make a diagnosis. Usually, the diagnosis is made by doing thorough history, examination and using standardized checklists completed by parents and teachers. Some children need behavioral modifications, therapy, and/or counseling. Some children additionally need medication to address their behaviors. Stimulant medications (Amphetamine, Methylphenidate) are the treatment of choice. There are other medications which can be used as either alternatives or in combination. There is evidence of some benefit of omega 3 fatty acid supplementation.
Tics and Tourette syndrome: Tics are sudden twitches, movements, or sounds that people do repeatedly.
Children who have tics cannot stop their body from doing these things.5 For example, a child with a motor tic might keep blinking eyes over and over again, nose twitching, head jerking or frequent shrugging the shoulders. Or, a child with a vocal tic might make a grunting sound, frequent throat clearing, humming, or yelling out a word or phrase unwillingly. The tic disorders differ from each other in terms of the type of tic present (motor or vocal, or a combination of both). When child has more than 2 types of motor tics and one vocal tic over a year, it is called Tourette syndrome.
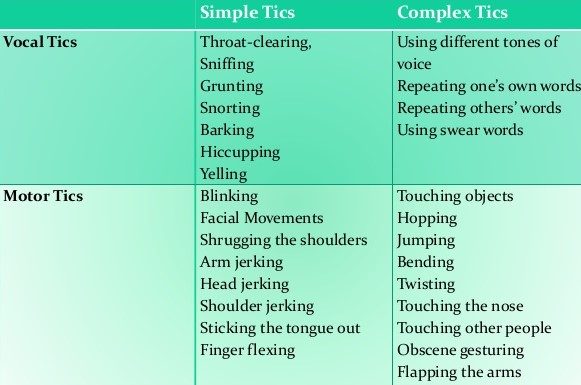
Tics typically show up between ages 2 and 15, with the average being around 6 years of age. Males are about three to four times more likely than females to develop Tourette syndrome. The exact cause is unknown. It is thought to be caused by a combination of inherited (genetic) and environmental factors. Chemicals in the brain that transmit nerve impulses (neurotransmitters), including dopamine and serotonin, might play a role. There is no specific test to diagnose it.
Tics can be suppressed for periods but are not under the full control of the person who has them. Tics will have a waxing and waning course. Strong emotional states such as stress or excitement often worsen tics. In mild cases, treatment is not necessary. Medications are available to control severe and interfering tics. Behavioral therapy including habit-reversal training can be useful. In some severe cases, Botox injections or deep brain stimulation (DBS) is used. Tics usually resolve by adolescence, but Tourette syndrome resolves by the age of 18 years only in 50% cases.
Cerebral palsy (CP): A group of disorders that affect a child’s ability to move and maintain balance and posture.
It is the most common motor disability in childhood. Cerebral (meaning to do with the brain) and -palsy (meaning weakness). It is caused by abnormal brain development or damage to the developing brain. It does not get worse over time. Symptoms can vary from child to child. Child with mild CP might walk a little awkwardly, but might not need any special help. On the other hand, child with severe CP might need to use special equipment to be able to walk, or might not be able to walk at all and might need lifelong care. Depending on the area of brain involved, there are 4 types of CP.
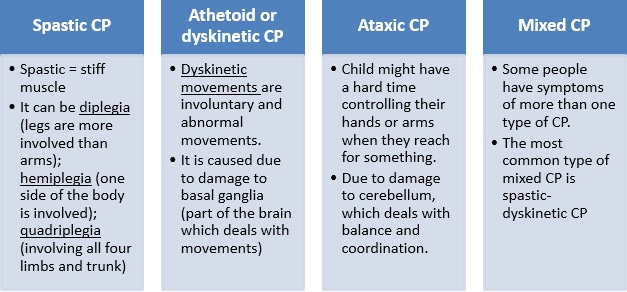
Diagnosis is mainly based on child’s symptoms, but he/she might need to undergo some blood tests and/or brain MRI. There is no cure for CP, but treatment can improve the quality of life. It is important to begin a treatment program as early as possible. Treatment methods such as physical therapy, occupational therapy and speech therapy help improve existing symptoms. In some cases, medications and surgery is needed.
Headaches: Among school age children ages 5 to 17 in the U.S., 20 percent (10.3 million) are prone to headaches. Headache can be from simple cold to brain tumor.
Tension headaches: The most common type of headaches is tension type headaches, followed by migraine headache. Tension headache is a band like head pain over forehead, pressure like in nature.
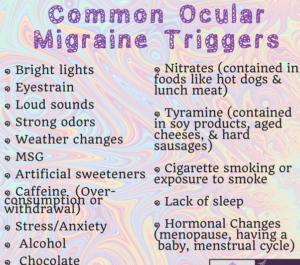
Migraine headaches: Migraine is a neurological condition, more than just a “bad headache.” Those who have these headaches might experience other symptoms beyond head pain, such as nausea, vomiting, dizziness, and mood changes, as well as sensitivity to light, sound, touch, and odors.6 Triggers can be skipping meals, dehydration, inadequate sleep, weather changes, hot weather, stress, some foods (MSG, chocolates, nitrates, nuts), perfumes, flashing lights, menstrual cycle in girls. Migraine can be with aura (aura is a warning sign that usually occurs before headache starts) or without aura. Most common auras are visual symptoms such as zigzag lines, blind spots, tunnel vision, flashing lights or sensory symptoms like pins and needle sensation in arm or legs.
There is a rare type known as migraine variant where headache might not be present but they have very different symptoms and usually present in young children. They usually outgrow or transition into classic migraine symptoms. Examples are: Cyclic vomiting syndrome, abdominal migraine, retinal migraine, ophthalmoplegic migraine, Alice in wonderland syndrome, Benign paroxysmal torticollis of infancy and acute confusional migraine.
Lifestyle modifications like good hydration, not skipping meals, good amount of sleep, keeping headache diary, identification and removal of any triggers, avoiding overuse of pain medication are very important aspects of the management. If needed, rescue medications like Acetaminophen, Ibuprofen, Naproxen or triptans can be used. If headaches are frequent and interfering, daily medications known as preventive therapy is used until child becomes headache free.
Muscular dystrophy: These are genetic (inherited) disorders of the muscles. Muscular dystrophy causes the muscles in the body to become very weak. The muscles break down and are replaced with fatty deposits over time9. There are 9 different types of muscular dystrophies and some types start in childhood age and some are adult onset.
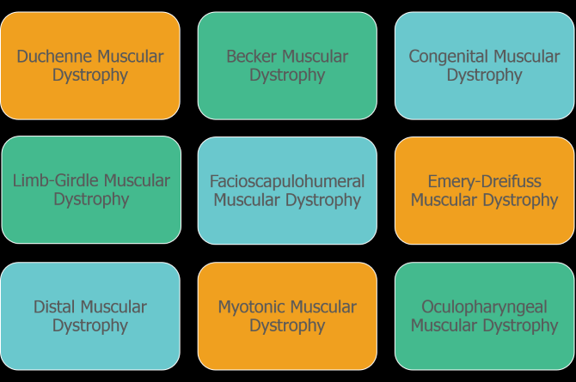
One group of conditions are known as congenital muscular dystrophies as well as congenital myotonic dystrophy are present at birth. Other types, known as Duchenne muscular dystrophy (DMD) and Baker’s muscular dystrophy (BMD) affect young children.
Early signs of the illness include a delay in walking, difficulty rising from a sitting or lying position, and frequent falling, with weakness typically affecting the shoulder and pelvic muscle as one of the initial symptoms. They might need tests like blood tests, muscle biopsy, electromyogram (EMG), EKG etc. BMD is a mild condition, but children with DMD become wheel-chair bound by the age of 12. They need physical therapy, medicines, braces, surgery depending on their symptoms.
Concussion/TBI: Concussion or mild traumatic brain injury (TBI) is an injury to the brain that results in temporary loss of normal brain function. It usually is caused by a blow to the head. In many cases, there are no external signs of head trauma.7
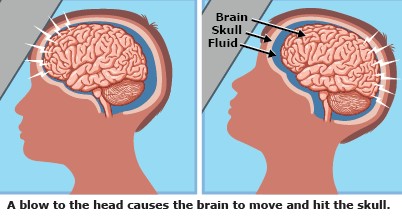 Many people assume that concussions involve a loss of consciousness, but it occurs in less than 10% cases. The old belief, called the Kennard Principle, that children who sustained a brain injury would heal quicker and more completely than adults who had sustained similar injuries, is not true. The younger the age of child, the more vulnerable brain is to concussion. Concussion can be due to fall, motor vehicle accidents, assault, child abuse, sports etc. Children can experience wide range of symptoms like headache, vomiting, dizziness, light sensitivity, memory lapse, balancing problem, sleep disturbances, focusing issue, mood changes, feeling of sadness, low energy level, vision problems, depression etc.
Many people assume that concussions involve a loss of consciousness, but it occurs in less than 10% cases. The old belief, called the Kennard Principle, that children who sustained a brain injury would heal quicker and more completely than adults who had sustained similar injuries, is not true. The younger the age of child, the more vulnerable brain is to concussion. Concussion can be due to fall, motor vehicle accidents, assault, child abuse, sports etc. Children can experience wide range of symptoms like headache, vomiting, dizziness, light sensitivity, memory lapse, balancing problem, sleep disturbances, focusing issue, mood changes, feeling of sadness, low energy level, vision problems, depression etc.
Here is a link to an interview I did about common myths about concussions in kids:👇
https://www.hackensackmeridianhealth.org/HealthU/2019/03/28/common-myths-about-kids-and-concussions/
After identifying the concussion, children should have strict brain rest (no screen, no studies, no exertion) for first 48 hours, that helps to recover brain faster. Child’s school, parents and his/her doctor should work together to help child slowly regain full brain functioning. School can provide accommodations (like 504 plan, IEP/individualized education plan or home instructions). Children take anywhere from 2 weeks to 3 months to recover completely.
Some children need medication to address headaches, sleep problems, focusing issue or depression. Depending on their symptoms, they might benefit from physical therapy, occupational therapy, speech therapy, cognitive therapy, vision therapy, vestibular therapy and neuropsychological evaluation. If child gets second concussion while recovering from the first one, it is known as second impact syndrome and it can be very dangerous.
Congenital brain malformations:Children are born with brain malformations if there are any problems in how the brain forms or develops. Folic acid deficiency in pregnant mothers can increase the risk of brain malformation. Hence, Centers for Disease control (CDC) recommends 400 micrograms of folic acid daily starting at least one month before pregnancy as well as during pregnancy. Other risk factors are use of alcohol, smoking, prescription drugs, recreational drugs, infections, exposure to X-rays, trauma during pregnancy. Healthy weight, blood sugar control before or during pregnancy if diabetic and avoiding taking any medications or herbal products during pregnancy is advised. There are many different types of brain malformations and children can have developmental delays, low IQ, seizures and other issues.

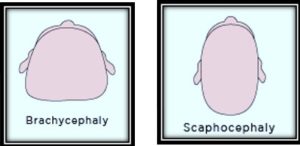
Head shapes: Flat head syndrome or plagiocephaly: Plagiocephaly (sometimes called deformational plagiocephaly or positional plagiocephaly) is a very common, very treatable disorder. Plagiocephaly develops when an infant’s soft skull becomes flattened in one area, due to repeated pressure on one part of the head. Many babies develop plagiocephaly by sleeping regularly in one position. In the 1990s, the American Academy of Pediatrics (AAP) introduced the Back to Sleep campaign, which urged parents to put infants to sleep on their backs successfully reducing Sudden Infant Death Syndrome (SIDS) by more than half.11
While the AAP still recommends back-sleeping to prevent SIDS, they have since recognized a correlation between back-sleeping and plagiocephaly. Mild cases of plagiocephaly can be managed by repositioning techniques and physical therapy. In severe cases, the custom cranial helmet can can be indicated to redirect baby’s natural growth into a normal head shape.
Other deformities are: brachycephaly (head is wider than normal) and Scaphocephaly (head is longer and narrower than normal).
Problems with head size:
Microcephaly (smaller head size),
Macrocephaly (larger head size)
The maximum growth of child’s brain happens in first two years of life.Hence, measurement of head circumference is very important to keep track of child’s brain growth. Head circumference is a measurement of a child’s head around its largest area.
It measures the distance from above the eyebrows and ears and around the back of the head. Pediatricians or family physicians measure child’s head circumference during regular visits and standard head circumference charts are used to keep the track.
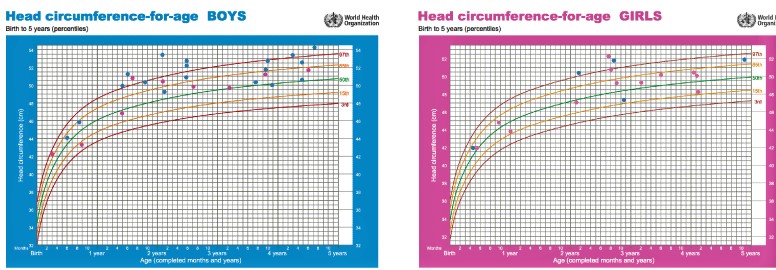
Macrocephaly means abnormally large head size and it is defined as head circumference more than 2 standard deviation (SD) on the growth chart. It can be due to thick skull bone, enlarged brain tissue (which could be due to some genetic conditions, accumulation of abnormal metabolic products), brain tumors, accumulation of brain fluid (called as hydrocephalus)
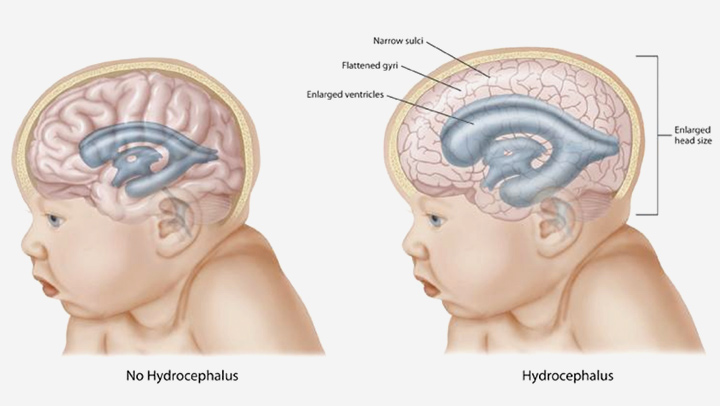
or accumulation of blood (subdural hematoma), infections (pus collection) or blood vessel abnormalities (arterio-venous malformations). In some cases, it is non harmful and the condition runs in the family. It is known as familial macrocephaly.
If child’s head in growing very fast and if he/she has vomiting, irritability, sleep disturbances, seizures etc, child needs urgent neurological evaluation.
Microcephaly means small head size and it is defined as head circumference less than 2 standard deviation on growth chart. However, there are some controversies about the definition. The causes can be genetic, brain injury during pregnancy (alcohol, drugs, infections, trauma), brain injury after birth (strokes, infections of brain and trauma) and some metabolic conditions. Marked slowing or arrest of head growth offers a poor prognosis for mental development.
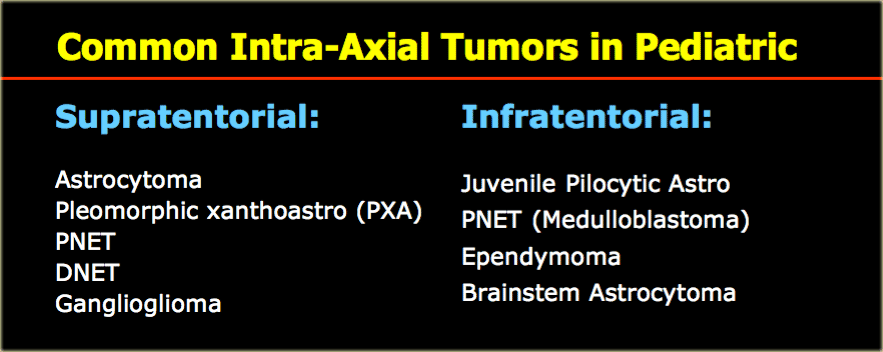
Brain tumors: More than 28,000 children (0-19 years of age) are estimated to be living with a brain tumor in the US.8
The most common types of brain tumors are: Pilocytic Astrocytoma, Malignant Glioma, Medulloblastoma, Neuronal and mixed neuronal-glial tumors and ependymoma. Children may present with headaches, balancing problem, seizures, vomiting, hormonal abnormalities, vision changes etc. Brain or spine MRI and other tests are helpful for the diagnosis. Sometimes, biopsy is needed. Treatment includes a multimodal approach of surgery, radiation therapy, and chemotherapy.
Neurocutaneous syndromes: These conditions have involvement of brain and skin (along with other organs in some conditions) due to common fetal origin. These are lifelong conditions and genetic in nature. Each disorder has different combination of symptoms ranging from tumors, skin lesions, seizures, hearing loss, developmental problems). Most of these conditions are inherited.
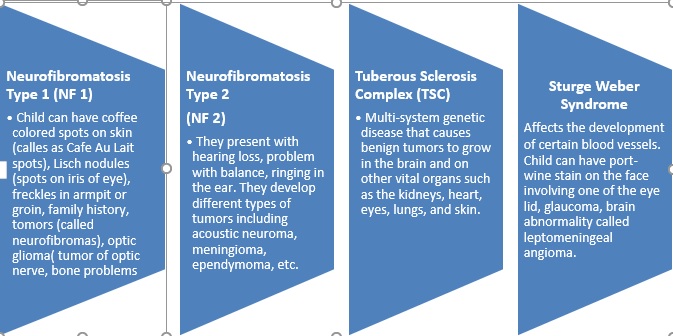
Other conditions are: ataxia-telangiectasia (A-T), von Hippel-Lindau disease (VHL), Incontinentia pigmenti, Hypomelanosis of Ito, PHACE syndrome etc.
Spinal Muscular Atrophy (SMA):It is a genetic disease affecting nerve cells (called as motor neurons) located in the spinal cord which controls voluntary muscle movement.
Atrophy means muscles get smaller when they are not active for long time. SMA is caused by genetic defect in the survival motor neuron 1(SMN1) gene on Chromosome 5.
Depending on the age of onset, there are 4 types:
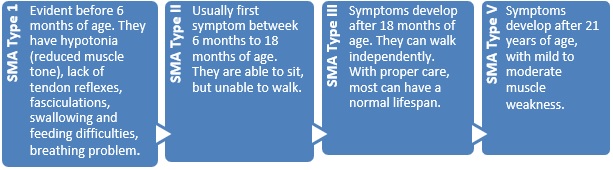
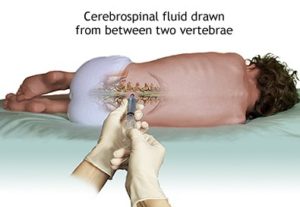
There are blood test/genetic test available for the diagnosis. There was no treatment available until 2016. In December 2016 the U.S. Food and Drug Administration (FDA) approved nusinersen (Spinraza) as the first drug approved to treat children and adults with SMA.10 The drug is administered by injection into the fluid surrounding the spinal cord. It is designed to increase production of the full-length SMN protein, which is critical for the maintenance of motor neurons.
Other pediatric neurological conditions are:
- ØPseudo tumor cerebri (Idiopathic intracranial hypertension),
- ØMetabolic disorders (huge number of inherited metabolic disorders),
- ØLeukodystrophies (inherited conditions affecting white matter of brain),
- ØStrokes in children,
- ØLearning disabilities including dyslexia,
- ØAutoimmune problems that impact the brain and spinal cord (such as multiple sclerosis),
- ØInfections or inflammation of the brain (such as meningitis or encephalitis),
- ØHydrocephalus (buildup of fluid in the brain)-they need VP shunt
- ØArnold Chiari malformation
- ØBrain aneurysms
- ØOther Genetic conditions
Child neurologists often make a diagnosis by hearing about your child’s symptoms, their medical history, and physical exam, but at times, more tests are necessary to make a diagnosis.
EEG (electroencephalogram) is a test that looks for problems with the electrical activity in your brain. This test can be used to look for seizures, and to make sure your child’s brain is making the expected types of electrical activity for their age. This test can be done as one hour test in outpatient setting, prolonged (48-72 hours) Ambulatory EEG (AEEG) as home test or inpatient prolonged (48-72 hours or more) Video EEG (VEEG).
MRI (magnetic resonance imaging) or CT scan are types of imaging tests used to take pictures of the brain and/or spine. These can look for signs of brain tumor, stroke, infection, multiple sclerosis, certain genetic conditions, and more.
Lumbar puncture (spinal tap) is a test where doctors insert a small needle in the lower back to take a sample of spinal fluid, which surrounds your brain and spinal cord. This can help look for signs of infection or inflammation.
Blood tests may be ordered for your child. These may include basic labs checking for electrolyte changes or signs of infection, or more complicated testing such as genetic tests for specific disorders.
References:
- https://www.hopkinsmedicine.org/neurology_neurosurgery/centers_clinics/epilepsy/epilepsy-in-children.html
- https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Febrile-Seizures-Fact-Sheet
- https://www.webmd.com/parenting/baby/intellectual-disability-mental-retardation#1
- https://chadd.org/about-adhd/overview/
- https://www.cdc.gov/ncbddd/tourette/diagnosis.html
- https://www.mdlinx.com/neurology/top-medical-news/article/2019/07/22/7573241?uic=ZZ2B8D7CBEB32E4B168BB0D0983BAD913B&utm_source=Sailthru&utm_medium=email&utm_campaign=Neuro%20Morning%20July23&utm_term=Daily%20Update%20Neurology%20With%20SailthruActivity
- https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Concussion
- https://braintumor.org/brain-tumor-information/brain-tumor-facts/
- https://childrensnational.org/visit/conditions-and-treatments/movement-disorders/muscular-dystrophies
- https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Spinal-Muscular-Atrophy-Fact-Sheet
- https://www.cranialtech.com/plagiocephaly/what-is-plagiocephaly/







Very informative article.So many new things explained in very simple language.Aunty keep up your wonderful act of knowledge sharing it’s very helpful for parents 🙏
Thank you, Mamatha 🙂
This was such a well written and very informative article . Thank you for sharing Dr. Savitra. I learned so much about the conditions pediatric neurologist treat.
Hello have a question
Sure. You can ask here or call my office.